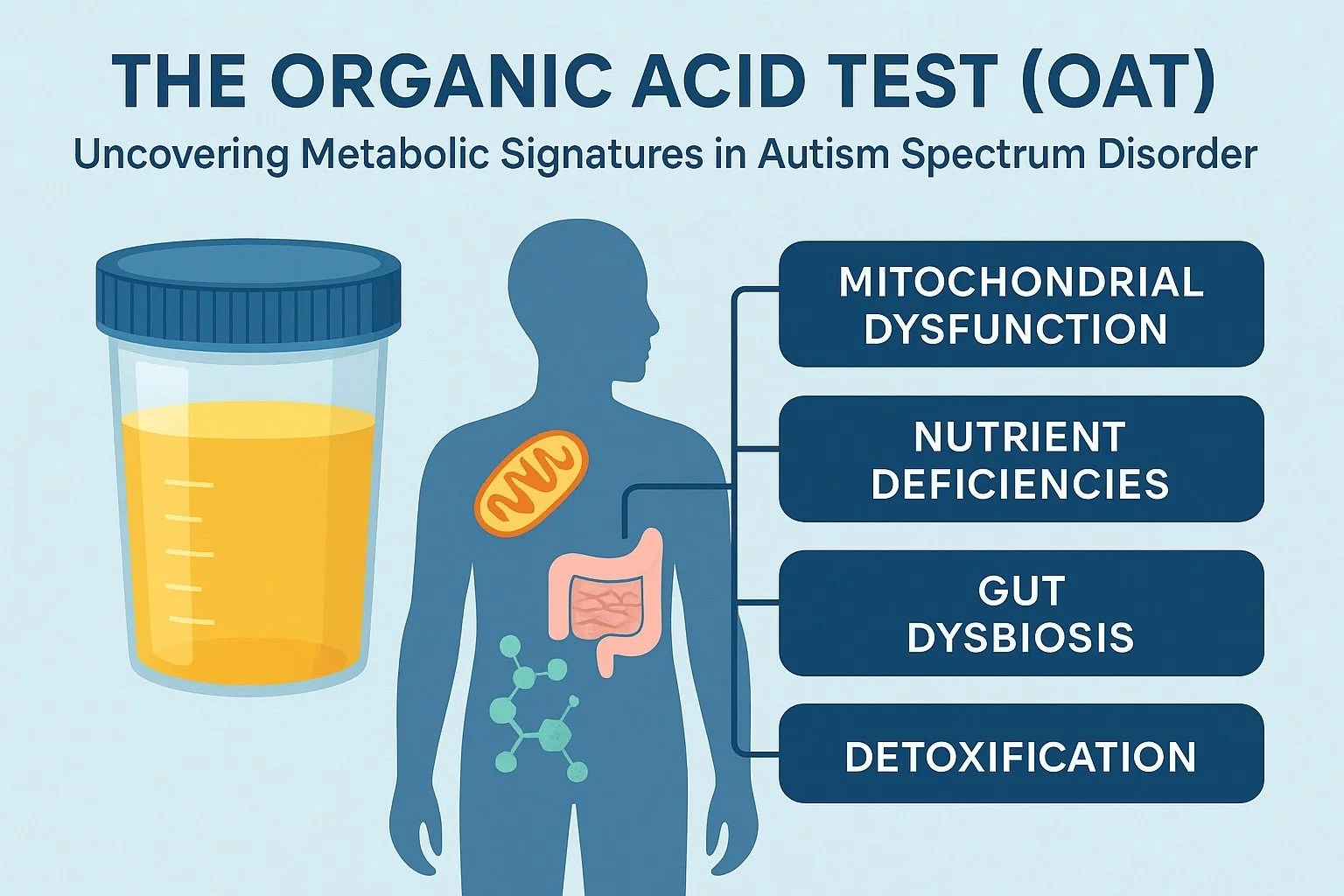
How the Organic Acid Test (OAT) Uncovers Hidden Metabolic Signatures in Autism Spectrum Disorder
Autism Spectrum Disorder (ASD) is complex, multifactorial, and uniquely expressed in each child. While behavioral assessments remain the foundation of diagnosis, many families today seek deeper insight into the why — the underlying biochemical imbalances that influence mood, behavior, attention, and overall development.
One functional medicine tool that has gained tremendous attention is the Organic Acid Test (OAT). When used thoughtfully in autism, the OAT helps uncover hidden metabolic signatures — such as mitochondrial dysfunction, nutrient deficiencies, detoxification stress, and gut microbial imbalances — that often go unseen on routine labs.
If you’ve searched for “OAT autism biomarkers” or “organic acids and autism,” this guide will help you understand what the test measures, how to interpret it, and how it can support a personalized, root-cause approach to healing.
1. What Is the Organic Acid Test (OAT)?
The Organic Acid Test is a comprehensive urine analysis that evaluates over 70 organic acid compounds. These compounds are by-products of key biological processes — energy production, neurotransmitter metabolism, detoxification, nutrient utilization, and gut microbial activity.
Because these metabolites are excreted through urine, the test provides a powerful snapshot of how well your child’s metabolism and biochemistry are functioning at a cellular level.
In functional and integrative nutrition, the OAT is used to identify metabolic stressors contributing to symptoms like anxiety, hyperactivity, poor focus, mood swings, gastrointestinal issues, and sleep problems — common challenges for children with autism and ADHD.
2. Why the OAT Matters in Autism
Children on the autism spectrum often exhibit imbalances that go far beyond the brain. Research has shown patterns of mitochondrial dysfunction, oxidative stress, detoxification challenges, and altered gut microbiota in many individuals with ASD.
The OAT test helps identify these patterns by revealing measurable metabolites that point to underlying dysfunctions, including:
Mitochondrial energy blocks that reduce ATP production and cellular energy
Oxidative stress markers indicating excess free radicals and low antioxidant capacity
Bacterial and yeast metabolites pointing to gut dysbiosis
Deficiencies in vitamins and cofactors such as B6, B12, folate, or biotin
Detoxification stress reflected by altered glutathione and sulfur metabolism
Understanding these imbalances allows for a personalized, root-cause plan — instead of a one-size-fits-all approach.
3. Key OAT Marker Categories in Autism (Explained)
The following are the most clinically relevant OAT marker categories often seen in children with autism, explained in clear terms.
Mitochondrial and Energy Production Markers:
These include metabolites like citric acid, fumaric acid, and aconitic acid from the Krebs (citric acid) cycle. When these are elevated, it can suggest mitochondrial stress or impaired ATP production — meaning the cells aren’t efficiently creating energy. Support may include CoQ10, L-carnitine, riboflavin (B2), and other mitochondrial nutrients.
Neurotransmitter Metabolites:
Markers such as homovanillic acid (HVA), vanilmandelate (VMA), and 5-hydroxyindoleacetic acid (5-HIAA) provide clues about dopamine, norepinephrine, and serotonin metabolism. Abnormal levels may indicate neurotransmitter imbalances, which can affect mood, focus, and sleep. These pathways rely on cofactors like vitamin B6, folate, and BH4 (tetrahydrobiopterin).
Oxidative Stress and Detoxification Markers:
Compounds like pyroglutamic acid and oxalic acid are related to glutathione recycling and oxidative stress. Elevated levels often mean the body is under toxic or oxidative load — which can occur with heavy metals, environmental exposures, or poor detoxification capacity. Support involves sulfur-containing nutrients (N-acetyl cysteine, glycine, taurine) and antioxidant support (vitamin C, alpha-lipoic acid).
Microbial and Yeast Metabolites:
OAT can detect gut dysbiosis through markers like arabinose, hippurate, and DHPPA. Elevated arabinose is often associated with yeast (Candida) overgrowth, while abnormal bacterial metabolites may signal an imbalance in the gut microbiota. Addressing these findings may include probiotics, antimicrobial herbs, or antifungal protocols under practitioner guidance.
Vitamin and Cofactor Markers:
Certain organic acids act as indirect indicators of nutrient status. For example, methylmalonate reflects vitamin B12 activity, xanthurenate reflects vitamin B6 metabolism, and 3-hydroxypropionate reflects biotin. Elevated levels can indicate a deficiency or impaired utilization of those vitamins. Correcting these cofactors helps optimize neurotransmitter synthesis, methylation, and overall metabolism.
4. Case Example: How the OAT Changed One Child’s Plan
Case:
An 8-year-old boy diagnosed with ASD presented with mood instability, speech delay, constipation, and significant sensory behaviors. Standard labs (CBC, thyroid, vitamin D, and B12) were all within range.
OAT Results (selected abnormal findings):
Elevated fumaric acid and citric acid (mitochondrial dysfunction)
High pyroglutamic acid (glutathione depletion)
Elevated arabinose (yeast overgrowth)
Elevated methylmalonate (B12 deficiency)
Elevated oxalic acid (possible gut or metabolic stress)
Interpretation and Plan:
Mitochondrial Support: Added L-carnitine, CoQ10 to support cellular energy.
Glutathione & Detox: Introduced N-acetyl cysteine and sulfur-rich foods for glutathione regeneration.
Gut Balance: Implemented a low-sugar, anti-yeast diet with Saccharomyces boulardii and specific probiotics.
B12 & Methylation: Added methylcobalamin (B12) and folinic acid to support methylation and neurotransmitter balance.
After three months, his energy, focus, and digestion improved. At six months, a repeat OAT showed normalized yeast markers and improved mitochondrial function.
5. Using the OAT Practically: A Step-by-Step Approach
Start with a Baseline OAT Test: Collect a first-morning urine sample following instructions carefully.
Interpret in Context: Review results with a functional medicine practitioner familiar with pediatric OAT interpretation.
Prioritize the Big Findings: Begin with key imbalances most connected to your child’s symptoms — such as yeast overgrowth or oxidative stress.
Support the Foundations: Focus first on clean, anti-inflammatory nutrition, mitochondrial support, and restoring gut health.
Address Detoxification Gradually: Never “push” detox — build from a strong foundation of hydration, antioxidants, and liver support.
Track Progress: Reassess symptoms monthly and repeat the OAT every 6–12 months to evaluate changes.
Adjust as Needed: Use follow-up results to fine-tune nutrients, probiotics, or detox supports.
6. Limitations and Considerations
The OAT is powerful, but it’s not a diagnostic test. It provides metabolic clues. Some key points:
Results can fluctuate based on diet, hydration, and medication.
Slight elevations are not always clinically significant.
Interpretation requires context: It should be evaluated alongside symptoms, other labs, and diet.
Cost: Often out-of-pocket, though sometimes reimbursable through health savings accounts.
When interpreted correctly, the OAT can reveal root causes and empower families to make targeted, evidence-informed changes.
7. Optimizing OAT-Based Interventions for Autism
Focus on whole-food nutrition: eliminate processed foods, dyes, and excess sugar.
Support gut balance first before layering detox or mitochondrial therapies.
Introduce one supplement at a time to monitor tolerance.
Encourage gentle detox pathways (Epsom salt baths, hydration, fiber).
Collaborate with a trained practitioner who understands both the science and individuality of each child.
Families often find that once metabolic stressors are addressed — through restoring nutrient sufficiency, balancing gut microbes, and supporting detoxification — children experience meaningful improvements in focus, mood, language, and behavior.
References
Frye, R. E., & Rossignol, D. A. (2011). Treating mitochondrial dysfunction in autism spectrum disorder. CPT: Pharmacometrics & Systems Pharmacology.
Filipek, P. A., & Jashar, D. (2019). Metabolic and mitochondrial dysfunction in autism spectrum disorders: A review. Journal of Autism & Developmental Disorders.
Naviaux, R. K. (2013). Metabolic features of the cell danger response. Mitochondrion.
DeFelice, T., & Bergin, A. (2018). Functional metabolic testing (OAT) in autism: Clinical application and limitations. Integrative Pediatrics.
Polk, R. E., et al. (2020). Urinary organic acids as biomarkers of mitochondrial dysfunction in ASD. Journal of Clinical Biochemistry.
Mosaic Diagnostics. The Organic Acids Test (OAT). Accessed 2025.